Since doctors confirmed the first cases of the coronavirus in the United States, health care workers, hospital administrators and politicians have been scrambling to procure ventilators to help COVID-19 patients who experience severe respiratory illness. In response to concerns of a shortage, Dr. Charles Robertson, an assistant professor of anesthesiology at the University of Mississippi Medical Center (UMMC), said he decided to build “the cheapest functioning ventilator” possible for use in extreme situations.
“My goal in designing this ventilator was to build the absolute minimum that I would need a ventilator to do, and it was to help other people,” Robertson said.
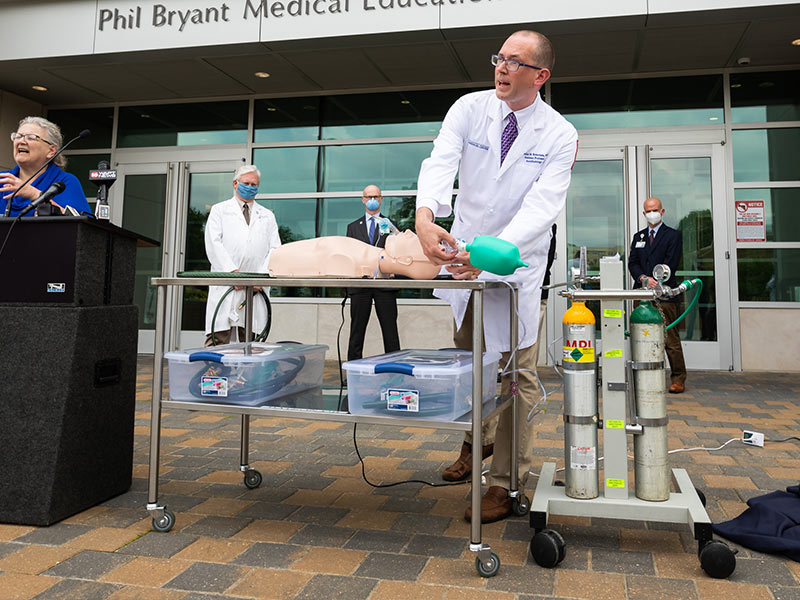
The Robertson ventilator is constructed from garden hose sections, adapters, valves, an electromagnet coil and a lamp timer, all of which can be purchased at any hardware store. Robertson said he got the total cost for his makeshift ventilator down to $50, and it can be assembled in under an hour.
The Institute for Health Metrics and Evaluation estimates that Mississippi will need 101 “invasive ventilators” at the peak of the pandemic, and the UMMC alone currently has 150 conventional ventilators in supply and 170 of Robertson’s ventilators constructed.
Though Mississippi is not one of the states likely to experience a shortage, others like New York and California have already requested federal supplies of ventilators, and these are examples of places where Robertson thinks his ventilator could help.
Even with an ample supply of ventilators, though, the survival rate of coronavirus patients who go on ventilators is exponentially lower than those who do not.
Dr. William Edmonson, a pulmonologist in Tupelo, said that he and his colleagues across the state do not feel an imminent threat of a ventilator shortage, but they have noticed that once a COVID-19 patient is on a ventilator, it is difficult to get them off.
Coronavirus patients who are likely to need a ventilator are those who develop acute respiratory distress syndrome (ARDS). However, Edmonson said that coronavirus patients do not follow the usual progression of symptoms that ARDS patients have.
“Normally, with just an average ARDS patient, you can get them off of the ventilator 80, maybe 70% of the time, and for this COVID stuff, it’s just the opposite,” he said. “They get stuck on the ventilator 70 to 80% of the time.”
Michael Dowling, the CEO of New York healthcare provider Norwell Health has estimated similar survival rates for coronavirus patients on ventilators, and the Associated Press reported last week that some doctors around the country are beginning to avoid the use of ventilators in treating coronavirus patients because of the low chance of survival after they begin treatment.

Robertson said his ventilators should only be used if “every single hospital ventilator is in use, and we have patients that are about to die because of that.” In these cases, Robertson envisions his invention being used as “bridge therapy,” meaning that the makeshift ventilator would only be in use until a conventional one becomes available to the hospital.
The prototypes of the ventilator underwent testing in the UMMC simulation laboratory and on laboratory animals, but it has not yet been tested by any outside entity.
“It’s reasonable to say this is not the sort of testing that we would see for medical devices in normal circumstances,” Robertson said.
Dr. Richard Summers, UMMC associate vice chancellor for research, said that since the ventilators have passed the hospital’s tests, UMMC is seeking federal authorization to use them in cases of emergency. Once that is granted, the design could potentially help other hospitals that are currently experiencing shortages.
“We have filed for an Emergency Use Authorization with the U.S. Food and Drug Administration who have indicated their interest in these ventilators,” he said. “I think this effort represents the independent ‘can-do’ attitude and ingenuity of our physicians and scientists to confront this crisis in the service of the people of Mississippi.”












